News
COVID inquiry: 'Why were RCN warnings ignored?'
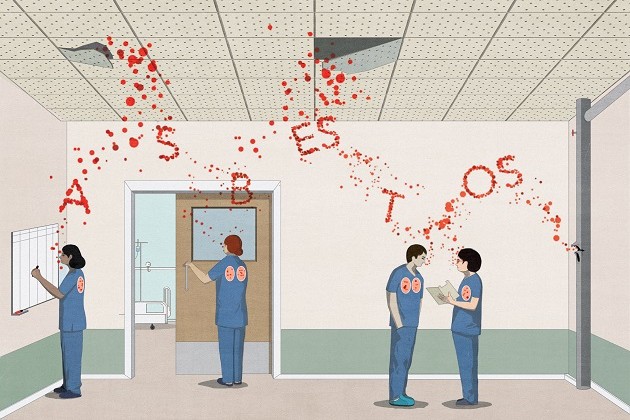
Nursing testimony at the COVID-19 Inquiry has highlighted how the failure to listen to the nursing profession led to inadequate infection prevention guidance and improper supply of PPE, putting staff at risk.

Connect with us:
Warnings from the nursing profession about the airborne transmission of COVID-19 were ignored for over a year by the UK government, a failure which “ultimately cost nursing professionals their lives”, the RCN has told the COVID-19 Inquiry.
UK-wide infection prevention and control (IPC) guidance predicated on droplet transmission went largely unchanged for 15 months, despite growing international evidence to the contrary. Repeated letters, emails and phone calls from the RCN about how the virus was spreading were ignored at the time.
When IPC guidance was being created, it was “critical for those who actually needed to use the guidance and implement it… to be involved,” the RCN’s Rose Gallagher MBE told the inquiry.
Rose, a specialist nurse and IPC expert advisor to the RCN during the pandemic, said that despite this: “As the largest part of the workforce, using the most PPE, we weren’t engaged with.”
Yesterday (5 November) Rose appeared as a witness in Module 3 of the COVID-19 Inquiry to answer questions about her previously submitted witness statement.
She said: “The RCN, on behalf of hundreds of thousands of nursing staff, repeatedly raised concerns and provided detailed evidence about how the virus was spreading. Government agencies did not listen. This issue was compounded by the failure to provide enough or the right type of protection based on inadequate IPC guidance. These multiple failings amount to a betrayal of health care workers, a betrayal which ultimately cost nursing professionals their lives.”
The failure to utilise the expertise of nursing staff also led to confusion, fear and a confidence crisis among frontline workers. “Our members were seeing other nurses in other countries wearing respiratory protective equipment, whereas here they were offered primarily surgical face masks,” Rose said. “There was a lack of understanding on why the UK seemed to be taking a different approach.”
The RCN continued to push for changes to IPC guidance throughout the pandemic. As the pandemic progressed, more nursing staff contracted COVID-19 and many developed long COVID.
As the virus depleted the nursing workforce, it piled pressure on remaining staff. “Mistakes can be made if you are short-staffed, if you're looking after too many patients,” Rose said. “What hadn’t been taken into account was the state of the workforce. Our members told us they felt blamed for increasing rates of health care acquired infection… but they were decimated as a workforce.”
The public hearings for Module 3 of the COVID-19 Inquiry will run until 28 November. We’re presenting evidence as a core participant, as the inquiry examines the impact of the COVID-19 pandemic on health care systems in the 4 nations of the UK. The focus is on the governmental and societal response to COVID-19 as well as dissecting the impact the pandemic had on health care systems, patients and health care workers.
Patricia Temple, an RCN member who worked as a staff nurse on the cardiac care unit of an NHS trust during the pandemic, also appeared at the inquiry to answer questions about her witness statement and pandemic experience. Patricia described poor communication around PPE, and a lack of access to adequate PPE which she believes resulted in her catching COVID-19 in the workplace, an infection that developed into long COVID. Patricia highlighted the lack of support for nursing staff who contracted long COVID, with many being forced to leave the workforce, and made to feel “disposable”.
Speaking ahead of the inquiry, Patricia said: “Working as a nurse during the pandemic was one of the most difficult times of my professional career and has had a long-lasting and significant impact on both my personal and professional life.
“This inquiry is providing an important opportunity for nurses to be heard and I feel a deep sense of responsibility to ensure I help represent the voice of nursing staff. During this time, we were let down by the system, there were many shortcomings, systemic failures, and excuses for questionable decisions. It's important these experiences be shared and heard.
“Having been seriously ill with COVID and, subsequently, being diagnosed with long COVID, I’m also able to speak on behalf of those frontline workers who are experiencing this. For me, this was a life-changing and soul-destroying event, and my losses were many and various, some temporary and some more permanent. This, I am sure, applies to many nursing staff who, like me, have been faced with either major alterations to their working lives or with dismissal on the grounds of ill health.
“I do hope the lessons learned from all that has been seen and experienced during the pandemic will be used constructively for the future and that all the issues raised will be acknowledged and used to ensure the necessary systemic change. This is an ideal opportunity to get things right going forward.”
Despite most European countries and many countries globally classifying COVID-19 as an occupational disease, the UK government is yet to follow suit. Although this concern lies outside the remit of the inquiry, we're calling on the government to classify long COVID as an occupational disease and we wrote to the UK government last year on this issue.
Take the opportunity to have your say: share your experience of working throughout the COVID-19 pandemic with . There’s a where there is a nation-specific inquiry taking place.